Here is the second part of my post. This portion talks about how I processed and eventually came to terms with knowing that seeing my kids grow up is statistically not in the cards for me.
Coming back to the evening of September 11, 2019, the day I found out my cancer had spread to my bones, I reached out to a friend who also has breast cancer. Even though I called right before dinner, she took time away from her husband and two young kids to speak with me. I talked and cried. She listened compassionately and then reminded me of another friend of ours had Stage 4 breast cancer with a similar diagnosis to mine. Between the three of us, we talked and texted for hours that night.
Over the course of the next week, I spoke to my medical oncologist, my surgeon, was referred to a neuro-oncologist and had more scans than I can remember. I was started on a hormone therapy that made sure that my chemo-induced menopause continued for life. I also started on a second targeted therapy called Perjeta, which in combination with Herceptin, binds to the protein receptors of the breast cancer cells, preventing them from receiving growth signals.
Typically, someone diagnosed with Stage 4 breast cancer would not get a mastectomy. There were now questions as to whether or not my surgery would proceed as planned. However, new research indicates there may be an advantage to removing the primary source of the cancer. Two weeks later, I had my mastectomy and said goodbye to one of my breasts and 6 lymph nodes. Chemo had already taken away my hair, eyelashes and eyebrows, which are important to my appearance, but at least those grow back. My right breast, however, was gone forever. It’s a scar that reminds daily of how fragile my life is.
Even though family, friends and community members were helping me every step of the way, I still felt isolated and alone. I was terrified. My emotions were following the ups, downs and twists of the wildest roller coaster ride imaginable. One day I thought I was fine and coping well and the next day I was sobbing hysterically. Working with a counsellor from the Psychosocial Oncology team and my GP Oncologist, I slowly regained control of my emotions.
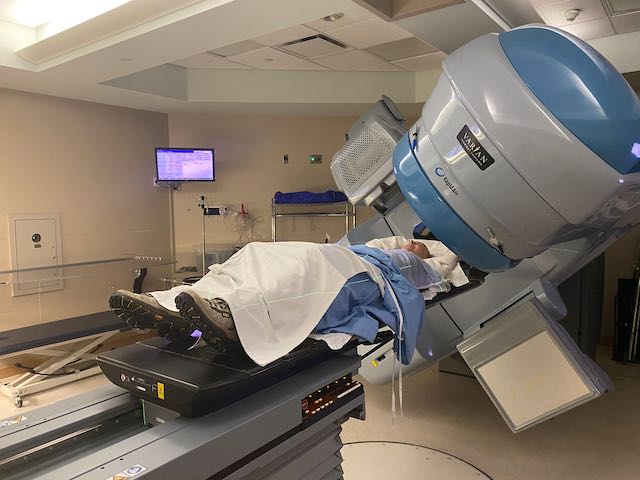
Next up was radiation. I thought chemo was hard, but I had no idea how debilitating radiation would be. My first round of radiation was delivered with a Linear Accelerator (LINAC), one of the most commonly used machines for external radiation therapy. By my third of my 16 radiation fractions of my treatment, I was sleeping between 12 to 14 hours a day. By the time I was done my treatment on December 10, almost three and a half weeks later, I was virtually bedridden. And, side effects hadn’t hit their peak. It usually takes approximately three weeks for the full effects to hit, which meant I spent Christmas and New Year’s in bed. [Read my blog “What I’m doing about the cancer Grinch who stole my Christmas” here.]
My time to recuperate was short. On January 3, 2020, I had the radiation mapping for my spine. Less than three weeks later, I underwent two fractions of Stereotactic Body Radiation Therapy (SBRT) to my T11 vertebral metastasis (mets). This is a relatively new type of radiation therapy, which delivers very high doses of radiation to specific tumours that are in difficult or hard to reach areas. Because a higher dose is used, fewer fractions are needed. Don’t be fooled! It doesn’t mean the side effects are any less miserable. While SBRT didn’t leave me with burned and bleeding scars like LINAC did on my chest, nor did leave my back “tanned” in the same was my face was after my chest radiation, it caused other side effects. With the dosage I received, I now have ~15% risk a spinal compression fracture to my treated vertebrae. I also experienced unbearable exhaustion.

Because I hadn’t been through enough, I still needed more treatment. A final palliative treatment that was added to my regimen in January was a bone metabolism regulator, given to me via IV infusion (just like chemo) every 12 weeks. This treatment aims to slow the destruction of my bones by the cancer and to reduce the speed of my morbidity progression. On one hand, I want to live as long as possible. On the other, it’s still hard for me to think that the longer I live with breast cancer, the more likely I am to have debilitating pain from the bone mets. I try not to think of my life in a long-term setting anymore. I have decided to look no further than 3 months out.
It took me 6 months to get through “grieving” my old life. It was only in March that I truly came to terms with the fact that I would never work or teach again, wouldn’t finish my second Master’s degree, nor do sports or travel as I did before. I reluctantly accepted that and that I possibly would not see my son turn 5 and most likely not see him turn 6. It became increasingly clear I have a limited time to spend quality time with my family and friends. My epiphany was that I need to do exactly that while I have my health. I’ve come to realize that I don’t know how I will feel or what I will be able to physically 6 or 12 months from now. Once I accepted this new reality, I was finally able to redefine how I fit into a world where my life had completely changed. Now that I am focusing on having meaningful experiences, I know I am building lifelong memories. That’s what drove my blog’s rebrand a few months ago.
Did you find the post useful for yourself or a loved one? If so, feel free to buy me a coffee or contribute towards some of my uninsured medical expenses.